If you and your partner are looking for a permanent form of birth control, you might want to consider getting a vasectomy.
What Is a Vasectomy?
A vasectomy is a permanent male sterilization procedure. The term “vasectomy” comes from the name of the tubes (vas deferens) in the scrotum that get cut during the procedure. This simple surgery can be performed by a doctor in an office, hospital, or clinic. The procedure is very quick, and you can go home the same day. A vasectomy is extremely effective in preventing pregnancy – almost 100%.
The Two Types of Vasectomies
There are two types of vasectomies commonly available: the conventional vasectomy and the no-scalpel vasectomy. Both procedures present minimal health risks.
1. Conventional Vasectomy
With the conventional vasectomy, your skin is cut so that the small tubes in your scrotum that carry sperm (vas deferens) can be accessed. The vas deferens tubes are cut or closed so that sperm cannot leave your body and cause pregnancy. The tubes and skin are then stitched closed and left to heal.
2. No-Scalpel Vasectomy
Instead of the skin being cut to access the vas deferens tubes, with a no-scalpel vasectomy, only a small puncture hole is made in the skin. The no-scalpel method lowers the risk of infection and other complications and generally takes less time to heal. Though the no-scalpel vasectomy can reduce complications, many men still have the traditional procedure done due to factors like cost and doctor preference.
The Effectiveness of Vasectomies
A vasectomy offers many advantages as a method of contraception. The main advantage is its effectiveness. Like a tubal ligation procedure for women, a vasectomy is a one-time procedure that provides permanent contraception. But when compared to a tubal ligation, a vasectomy is more effective, can be performed outpatient, is less complex, and often is more affordable
The main reason the vasectomy procedure is so effective is because it is designed with permanence in mind. Unlike other forms of contraception, a vasectomy is a long-term plan.
A vasectomy procedure is more than 99.9% effective in preventing pregnancies.
Although vasectomies are known for their effectiveness, it is important to bear in mind that it takes a considerable amount of time after the procedure for semen to be completely free of sperm. Everyone’s experience is different, but in some cases, it can take a few months to get sperm-free semen.
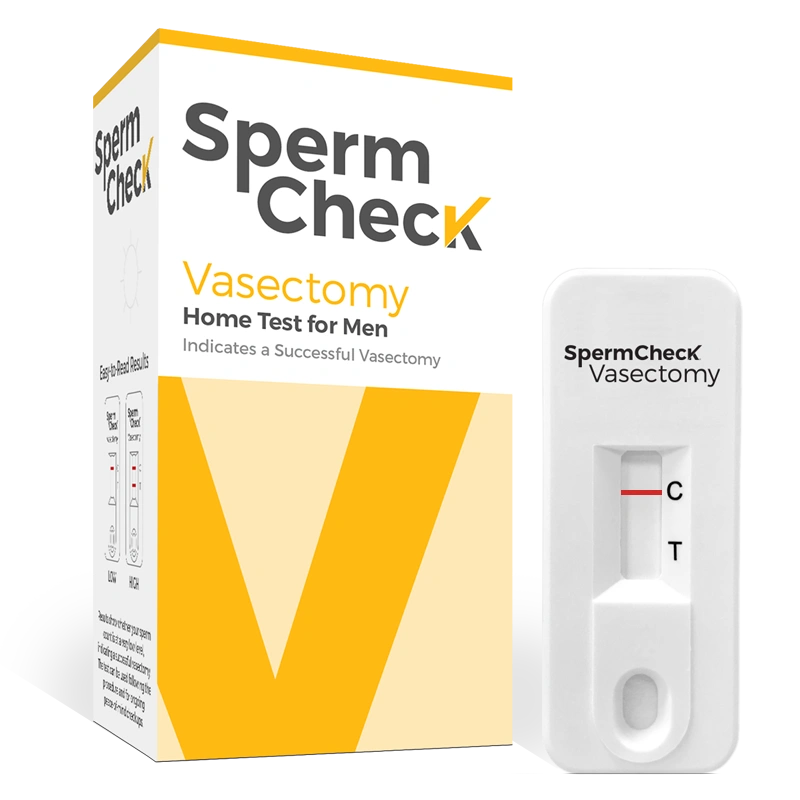
It is likely that two to three months after you have your vasectomy procedure, your doctor will ask you to come in and provide a semen sample that can be tested . It is best to avoid engaging in sex without another form of contraception until after you take this sperm analysis test and are assured by your doctor that there is no sperm in your semen. Don’t want to make the trip back to your doctor’s office? Test your sperm at home with SpermCheck Vasectomy.
Does Getting a Vasectomy Affect Your Testosterone Levels?
After a vasectomy, lower testosterone levels are uncommon. While sperm will no longer be present in your semen, all other components, including hormones like testosterone, will remain. Getting a vasectomy typically does not have a significant impact on male hormone levels like testosterone.
Testosterone production occurs within the testicles in response to signals from the pituitary gland. These signals are not disrupted by a vasectomy and the surgery does not interfere with the testicles’ ability to produce hormones. Healthy testosterone levels for adult men can fall anywhere between 300-1000 nanograms per deciliter (ng/dL).
Individual responses to the vasectomy procedure may vary, but it’s important to note that significant hormonal changes, such as lower testosterone levels, are rare. Most men do not experience any notable hormonal changes following the procedure.
Get Informed Before Your Vasectomy
Undergoing a vasectomy is not a decision to be made hastily. It’s important for both you and your partner to carefully evaluate if this is the appropriate choice for your situation. Vasectomies are intended to be permanent solutions. While a vasectomy reversal is possible, it can be challenging and is not always successful. The success rate for reversals varies by the method performed, but a typical vasovasotomy reversal procedure success rate is between 90-95%; however even with a successful reversal, there may still be difficulties in achieving pregnancy. A vasectomy should only be considered if you are completely certain that you seek a permanent form of contraception.
5 Common Misconceptions About Vasectomies
Common vasectomy misconceptions include:
1. It Takes a Long Time to Recover from a Vasectomy
Many people believe that the healing time after a vasectomy procedure is quite long, which is not the case for most people at all. Most people that undergo a vasectomy fully recover in about a week, returning to pain-free sexual activity.
2. Vasectomies Can Cause Erectile Dysfunction
Some men believe that vasectomies are linked to erectile dysfunction, which is not true; in actuality, vasectomies do not affect a man’s ability to achieve or maintain an erection. Erectile dysfunction is primarily related to factors such as blood flow, hormonal balance, psychological elements, overall health, and certain medical diagnoses, including prostate cancer.
3. A Vasectomy Is Extremely Painful
You can expect some discomfort and pain with almost any surgery, even those that are minimally invasive. With a vasectomy, this temporary discomfort is often the most pain a person will experience throughout the process. While some patients note feeling sensations of pressure, reports of extreme pain associated with a vasectomy are quite uncommon. Typically, over-the-counter pain medicine is more than enough to keep someone recovering from a vasectomy feeling comfortable.
4. Vasectomies Can Affect Your Sex Drive Long-Term
After you are fully recovered from your vasectomy, there should be no aspect of sexual function or sexual satisfaction that is hindered. Although it is important to note that you should still use a form of contraception until you and your doctor have tested and ensured your semen is free of sperm.
5. Vasectomies Are Unreliable
Post-vasectomy fertilizations are extremely unlikely. Although shortly after the vasectomy procedure, sperm cells can still be found in semen. This is why it is so important to have your semen tested. Once your doctor tests your semen and confirms there are no sperm cells present, the likelihood of egg fertilization is near zero. The best practice is to check your semen for sperm once a year to minimize the risk of pregnancy from post-vasectomy recanalization. Check out SpermCheck Vasectomy and get the answers you’re looking for from the comfort of home.
Potential Vasectomy Complications
Minor vasectomy complications can include:
Pain
Any procedure has the potential to cause pain, and in rare cases, residual pain may occur. Your testicles are sensitive organs, so temporary pain is not an uncommon occurrence. Very rarely, some men experience persistent pain after the procedure, called Post-Vasectomy Pain Syndrome.
Sperm Granuloma
You may notice that a hard and potentially painful lump in the testicles has formed. This lump is most likely a sperm granuloma. A sperm granuloma is caused by sperm leaking from the severed vas deferens. A sperm granuloma is not dangerous and is almost always absorbed by the body. Support for the scrotum and mild painkillers (such as acetaminophen) can relieve symptoms.
Want to make sure your vasectomy is still doing its job?
An at-home sperm test from SpermCheck can help you make sure your vasectomy worked (and keeps working). Order your SpermCheck Vasectomy test today.